Reclassification of opioid painkillers may boost workers compensation costs
As DEA changes rules on opioids, insurers must adjust Reprints
Tighter controls on opioid prescription painkillers issued by the U.S. Drug Enforcement Administration last month may increase workers compensation costs in the short term, but over the long term they could help reduce overuse of opioids.
The new regulations may drive up the price of some drugs and will force some workers comp claimants to visit their doctors more frequently to obtain prescription painkillers, increasing employer costs, but closer monitoring by medical professionals may lead to alternative therapies that don't rely on potentially addictive drugs, experts say.
Despite the tighter controls, opioid use by workers remains a critical workplace safety concern, they say.
Last month, the DEA said that effective Oct. 6, hydrocodone combination drugs — powerful opioids that have been prescribed increasingly over the past several years to treat injured workers — would be classified as Schedule II controlled substances under the federal Controlled Substances Act. Previously, they had been classified as Schedule III. Pure hydrocodone already was considered a Schedule II controlled substance, along with opioids such as oxycodone and morphine.
In addition, the DEA classified tramadol, another opioid painkiller but one that is generally viewed as less powerful than some others, as a Schedule IV drug last month. Previously, tramadol, which is sold under the names Ultram and Ryzolt, was unregulated by the DEA.
Under DEA rules, Schedule II drugs cannot be refilled under the same prescription, whereas Schedule III and Schedule IV drugs can be refilled up to five times, with prescriptions expiring after six months.
As an unregulated substance, patients had access to unlimited refills of tramadol over the course of one year in most states, said Paul Peak, pharmacist on the complex pharmacy management team at Sedgwick Claims Management Services Inc. in Memphis, Tennessee. However, at least 10 states treated products containing tramadol as controlled substances prior to the DEA's classification, Mr. Peak said.
As a result of the changes for both classes of drugs, some injured workers may have to make more frequent physician visits to be monitored or to obtain new written prescriptions, said Dr. Robert Hall, medical director at pharmacy benefit manager Helios, which formed from the merger of PMSI Inc. and Progressive Medical Inc., in Tampa, Florida.
“We are increasing costs to the system” by having injured workers visit physicians more often, but there's also a chance that those visits could lead to better care, said Brian Carpenter, senior vice president of pharmacy product development and clinical management at Healthcare Solutions in Atlanta.
“As long as the physician is ... checking to see if optimal capacity is increasing with the use of the drug, making sure there isn't aberrant behavior” and doing drug screenings, costs could actually decrease in the long run, Mr. Carpenter said.
However, if more claimants begin taking tramadol as a result of hydrocodone combination products becoming more controlled, the average wholesale price of tramadol products could increase, Dr. Hall said.
The DEA is “adding a lot more control,” but the controls are not as restrictive as those imposed on hydrocodone combination products, such as Vicodin and Norco, that can no longer be refilled under Schedule II, Mr. Carpenter said.
As tramadol is less tightly controlled than other popular opioids, its use may increase despite the tighter controls imposed on the drug because the alternatives are even more tightly controlled, experts say.
In October, claimants who were taking hydrocodone products may switch to tramadol or codeine, Mr. Carpenter said, although “a lot of users don't like codeine because it has more side effects.”
“It will be interesting now to see if codeine will be on the uptick because of the conditions that are being placed on the hydrocodone combo products,” Mr. Carpenter said.
Even though the DEA has tightened controls on tramadol and hydrocodone combination products, employers and third-party administrators “can't, in most situations, prevent someone from taking it unless an outside peer reviewer comes along and says it's not necessary,” Mr. Peak said.
And despite the tougher controls, employers with workers in safety-sensitive roles need to be aware that these opioids can cause sedation, he said.
Mary K. Schottmiller, senior labor and employment counsel at Prime Healthcare Management Inc. in Ontario, California, said it's not uncommon for nurses, for example, to take painkillers because of the work they do, but it's unclear what effect — if any — the new restrictions will have.
Barbara Back, director of human resources at Prime Healthcare Management's Encino and Sherman Oaks hospitals in Oxnard, California, said prescription pain medications are treated like alcohol and marijuana in the workplace.
“They could have the same outcome as if you were on an illegal substance,” Ms. Back said. “So even though it's a prescription, it would impair your physical ability and also your mental ability to perform work.”
Read Next
-
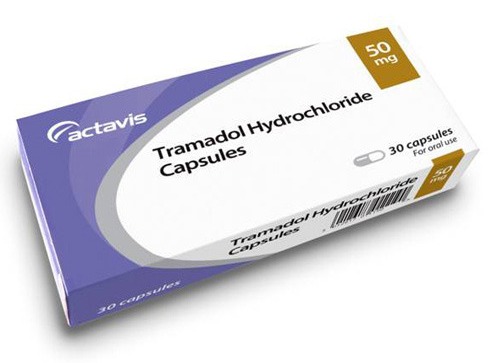
DEA reclassifies painkiller tramadol as a controlled substance
The U.S. Drug Enforcement Administration began labeling tramadol, an opioid pain medication, as a Schedule IV controlled substance on Monday, according to a final rule published in the Federal Register.